I have a lot to type
We made it to check in yesterday the 27th without any further changes or delay to the schedule. Brendan was in a good mood and charming all of the nurses with his big eyes and his smile. With each person that came in the room, he would ask, “Is this the person that is going to cut me open?”

I was happy that he could be silly.



Brendan selfies

After all the prep was done, they gave him some versed for the part where he had to leave us. The procedure went very well. The surgeon said that there were no surprises and everything was smooth.
He went straight to his room in the cardiac ICU. They were able to extubate in the OR and let him breath on his own. He was put on a little oxygen but his sats are in the high 90’s, even hitting 100!!! I really don’t know what to think about that. He may sit in the low to mid 90’s without oxygen, but this could get better over time. We have been telling Brendan that he was going to surgery to get upgrades so that he would feel better. He told the nurse he was getting a “running upgrade” so he could be as fast as Trevor.
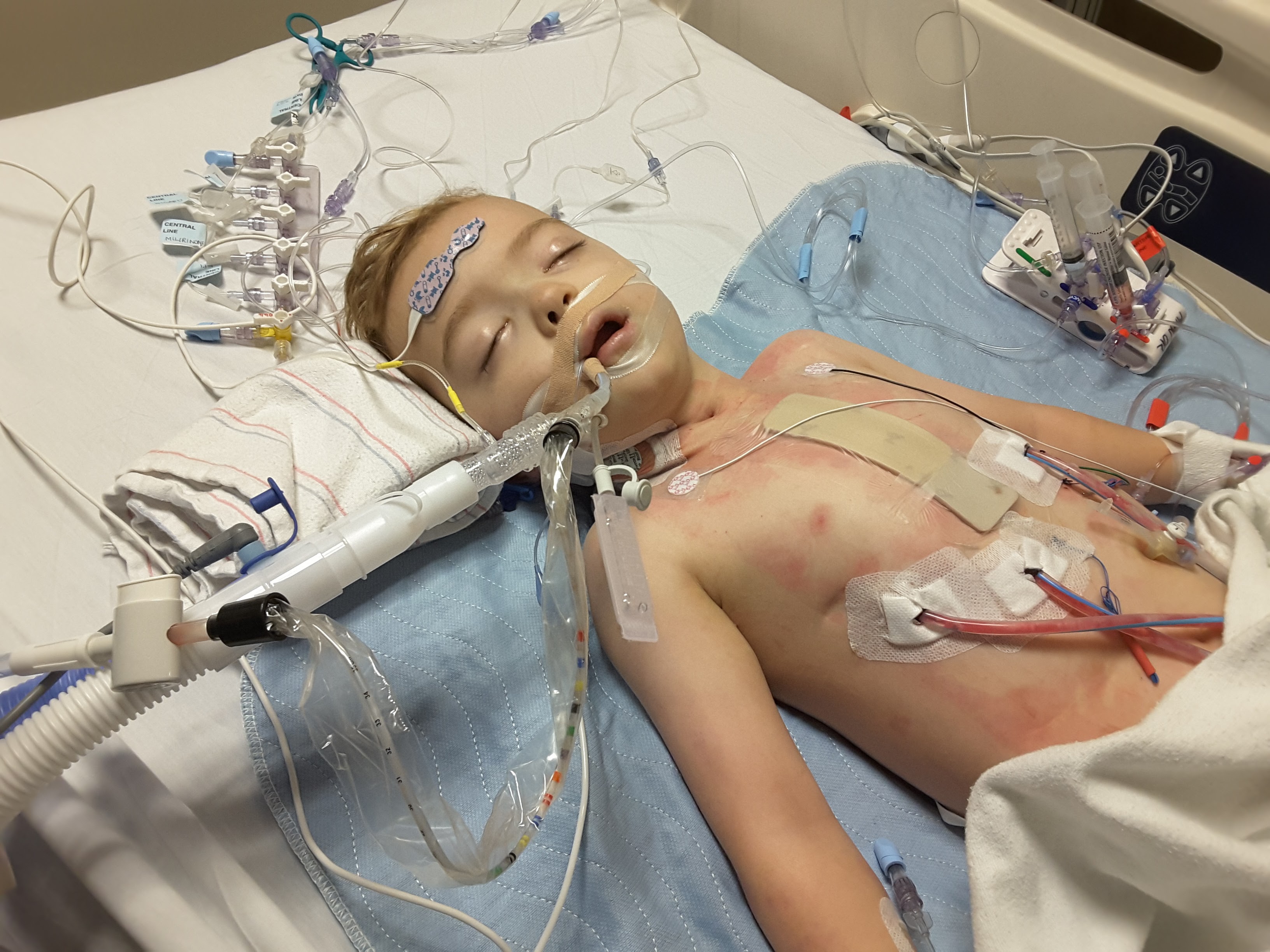
He has nine different IV pumps running. He is on dexmedetomidine for sedation, several saline pumps for keeping his lines flushed and open, some heart medications like milnarone for helping the heart with the changes to the physiology. He is getting morphine and ativan. He has an internal jugular central venous line in his neck, an atrial line in his left arm, an iv in his foot, an iv on his right arm, and three very painful large chest tubes draining the build up of fluid around his lungs. Even when sedated, if they touch the chest tubes, he winces and cries out through the sedation. His blood pressures stayed low, they give him blood and fluids to balance what he is losing through the chest tubes. Anyone that asks, “Is there anything I can do?”. Yes. GO DONATE BLOOD.



Throughout the afternoon and continuing all night, the right chest tube was draining blood. They have been using different medications to manage it. Some bleeding is expected because of the heavy blood thinners they used during surgery. By about 5am today, he had lost over a liter of blood and fluid through his right chest tube. He got blood, platelets, plasma, and cryoprecipitate as well as multiple calcium infusions but it drains as fast as they are putting it in. I heard the night nurse say to another that she gave Brendan more blood product last night than she has given total in the last two years.
The team was communicating with the surgeons through the night. They made the decision that it was necessary to take him back to the OR this morning. They are going to put him back under general anesthesia. They will reopen the same incision/no more cutting required. They are going to wash out his chest and remove all of the blood and fluid building up and locate the source of the bleeding.
Both the surgeons and Brendan’s cardiologist were explaining that kids with the Glenn surgery develop tiny collateral vessels or “accessories”. These are actual new abnormal blood vessels that grow between the aorta with the pulmonary arteries or other existing blood vessels. Like shortcuts. The heart is trying to find new pathways. The concept is amazing to me really.
During surgery, they cauterized and removed what they could find. They firmly believe that it is one of more of these tiny collaterals that is leaking and causing the internal bleeding. His fontan circulation is doing excellent, his sats are still excellent.
When he does wake up at all, he in in extreme pain. He yells “stop” and he wants to pull the dressings off of his chest.
At 8:00am AZ time, they took him back to the OR. The anesthesiologist just informed me that he will come back to the room still intubated with a ventilator. They will keep him that way for some time in order to verify that the bleeding has stopped for sure. They do not want to extubate again and then end up going back in again.
I was assured that this should not delay his overall recovery time. The opening is still so fresh, there should be no trouble getting into his chest. They expect that this will take about an hour to an hour and a half.
Trevor has been very emotional and confused by everything. He spent the afternoon yesterday with his friend Blake while Bill and I were with Brendan. He is at home with Bill this morning and Gramma will be flying in tonight to help take care of him. He has always been super sensitive and picks up on our emotions easily.
I will post here again when I have more news and time to update. Thank you everyone for the comments and support on facebook.
Brendan (and Trevor!) would love to receive mail. If you can send a postcard for the wall or a letter or drawing of encouragement, here is the info from the hospital web site:
“Friends and relatives who wish to send cards or gifts to the hospital should use this address:
Brendan Aylesworth
Phoenix Children’s Hospital
1919 East Thomas Road
Phoenix, AZ 85016
Mail and gifts are delivered to the child’s room. Due to certain health-related restrictions, latex balloons cannot be sent to the hospital. Intensive Care Units and the Hematology/Oncology Units do not allow the delivery of fresh flowers and/or balloons”
Brendan loves owls, ostriches, cockatoos and anything to do with Fantastic Beasts and Where to Find Them. Trevor loves soldiers, camouflage, Halo (video game), sea creatures especially stingrays and puffer fish. They both like ninjas and Minecraft.
We have had a really good team of nurses. All of the staff remember Brendan very well. They all adore him and are doing their best to keep him comfortable.